Cryptorchidism: the testicle not descended or hidden. Causes, symptoms and how it is treated
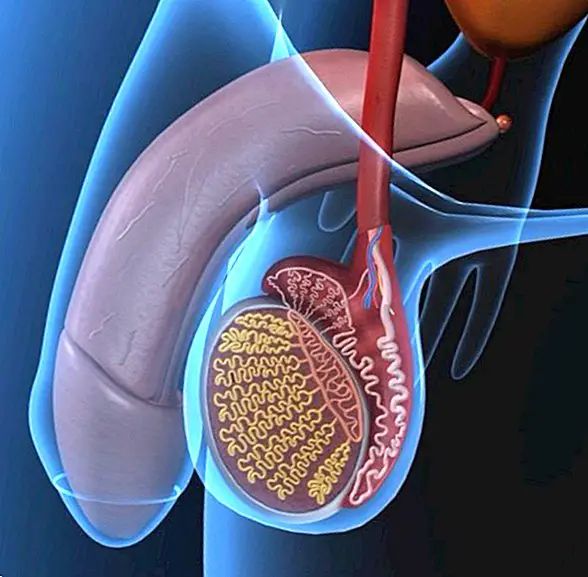
Cryptorchidism is a disorder medically known by the name of testicle not descendedor hidden testicle, and consists basically of an anomaly of congenital character, in which one or both testicles do not descend correctly. As a result, they tend to stay in the inguinal canal or abdominal cavity, not reaching down to the scrotum normally. In addition, the right testicle is usually the most affected.

It is, in fact, one of the causes that can cause sterility during adulthood, especially when it is not treated in time. Further, is a very frequent disorder in premature babies; that is, in children born before completing 37 weeks of pregnancy.
What is cryptorchidism?
It is a common alteration of the normal development of the testicles. It is estimated that between 1 and 3% of children born at term suffer from it, although in the case of premature births it tends to affect around 30% of babies. However, it is estimated that more than 95% of cases, throughout the first year of the child's life, the testicle tends to descend normally.
As we explained briefly at the beginning of this note, Cryptorchidism is the absence of one or both testes in the scrotum. That is to say, the testicle has not descended normally to the scrotum, so that it is 'hidden' in the abdominal cavity or in the inguinal canal.
There are two types of cryptorchidism:
- Unilateral cryptorchidism:It occurs when only one of the testicles has not descended correctly. It is the most common congenital malformation of cryptorchidism, accounting for 85% of cases. In fact, the right testicle is usually the most affected.
- Bilateral cryptorchidism:It occurs when neither of the two testicles descends normally to the scrotum. It is, in fact, a less common malformation than the unilateral one.

What are the causes of cryptorchidism?
There are several causes that can cause the testicle has not been able to descend to the scrotum normally. For example, it may be due to anatomical irregularities that interfere or block in the normal path that goes to the scrotal sac, or a hormonal alteration that prevents or delays the normal development of the baby.
In any case, below we explain what are the main causes of the undescended testicle:
- Genetic causes or chromosomal alterations: alterations in the Y chromosome, Klinefelter syndrome, Prader-Willi syndrome and Kallman syndrome, among others.
- Anatomical alteration.
- Mechanical obstacle - as we are going or spermatic nerves - that appears during the normal migration of the testicle.
- Very narrow inguinal canal.
- Defect or hormonal insufficiency: testosterone deficiency, AMH, hCG, LG or FSH, among others.
- Lack of intra-abdominal pressure.
How is it diagnosed in babies?
The most common is that the diagnosis is made after a palpation of the scrotal bag of the baby by the pediatrician, pediatric urologist or pediatric surgeon. This palpation can be carried out in the child at the time of birth or in some routine revision that is carried out later.
When one of the testicles - or both - is not located in the scrotum and therefore can not be found during palpation, the most common is to perform a abdominal ultrasound. And if finally with this medical test it is not possible to find them, other tests like the ultrasound to visualize the testicles in the inguino-scrotal tract, or a magnetic resonance.
How is it treated?
The most usual is to wait for the first year of the baby's life, since it is common for the testicle to descend spontaneously during the first 6-12 months of the child's life. However, when this does not happen, it is possible to opt for different treatments:
- Hormone treatment:It consists of the administration of hormones such as testosterone and beta-hCG, which stimulate the descent of the testes. If administered, it is necessary for parents to examine the baby periodically after the first month, then after six months and finally every year until reaching puberty. However, it is a treatment that is currently not widely used due to its side effects.
- Surgery:It is a surgery known as orchiopexy. It tends to be carried out before 2 years of age, and the sooner a better prognosis is achieved, since it will have a positive influence on fertility, the risk of testicular cancer will decrease and there will also be a greater recovery of testicular volume.

What are the consequences if it is not treated on time?
When the cryptorchidism does not correct itself, and also does not follow proper medical treatment in order to solve the problem, serious consequences may occur in the long run, since Testicular tissue is severely damaged when found in an abnormal position, that anatomically does not correspond to him. And what are these consequences ?:
- Sterility:It occurs when the testicular tissue has been damaged, so it is quite possible that the production of sperm in adulthood is little or no.
- Testicular torsion:It occurs when the spermatic cord undergoes torsion, interrupting the blood supply to the testicle.
- Testicular cancer:Due to an increase in temperature and an alteration in the normal development of the testicle, men with cryptorchidism have a higher risk of developing a tumor in the testicle.
- Inguinal hernia:It consists of the protrusion or exit of a part of the intestine through an opening found in the abdominal wall in the groin.
As we can see, if you have diagnosed your child with cryptorchidism recently in the first place you should not worry. The most normal thing is that the undescended testicle goes down to the scrotum during the first year of life. And, in case of not doing so, there are effective medical treatments that can be of great help. The key is to treat it as soon as possible, always following the advice of the pediatrician or the child urologist. This article is published for informational purposes only. You can not and should not replace the consultation with a Pediatrician. We advise you to consult your trusted pediatrician. ThemesInfertility